Ophy Care is filled with joy to announce its partnership with Palestine Children’s Relief Fund (PCRF) — a US-based nonprofit dedicated to providing medical relief to children in conflict.

Through the partnership, Ophy Care will provide its cutting-edge telehealth platform and EMR (electronic medical records) system to PCRF. The innovative tech solution will help PCRF carry out medical outreaches with greater consistency and conduct medical missions more effectively. PCRF would be able to do pre-mission screenings and post-mission follow-up visits through Ophy Care’s telehealth while managing all the patient data on a centralized EMR.
Why Ophy Care and PCRF are Joining Together?
Though PCRF and organizations like such are doing a pivotal job in healthcare provision to underprivileged and deprived parts of the world, such as Palestine, several barriers interfere with their mission. Distance and the excessive number of cases being the biggest challenges.
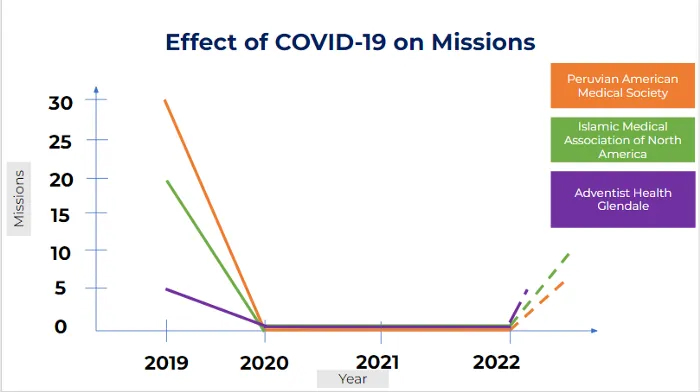
PCRF finances dozens of medical missions each year to send medical experts from all over the world to the Middle East and provide the locals with otherwise inaccessible healthcare. However, the problem is that sponsoring these medical missions can get very costly.

According to this study published in Globalization and Health, sending one physician or medical expert on a short-term medical mission can cost about $11,000. A short-term medical mission can last anywhere from a few days to a couple of weeks. However, most time is spent screening cases before performing the actual surgery.
The other big issue is that these missions are unable to perform post-surgery visits, which can cause more complications later on.
By shifting prescreening of patients and post-surgery visits to a virtual platform, not only can PCRF save a large sum of finances but also improves the successful and sustainable delivery of care.
Another problem that PCRF faces is managing the health data of thousands of children being treated by hundreds of doctors at different sites. Managing that data on paper is impossible. For this, PCRF required a centralized, easily manageable, and remotely accessible patient medical record management system.
Ophy Care’s telehealth software and EMR offer PCRF an ingenious solution to both of these problems.
“Organizations which are doing very critical work in conflict-hit countries with little to no resources need to be equipped with state-of-the-art tech solutions so they can utilize the little resources they have in a very efficient manner,” said Etizaz Shah — founder and CEO at Ophy Care.
How Ophy Care Offers a Solution to PCRF?
Ophy Care has developed a telehealth platform that allows medical organizations worldwide to improve healthcare equity by tackling spatial, linguistic, and cultural barriers, even in the most remote regions of the globe.
The bridge between a healthcare expert from a developed country like the United States and underprivileged patients in conflict-hit areas like Palestine is no longer a matter of thousands of dollars and weeks-long expeditions. Technologies like Ophy Care allow providers to connect with citizens of these deprived regions in the course of minutes without dedicating large portions of the budget to checkups.
Our software solution will enable PCRF to reduce the duration of medical missions without compromising on the quality of service. In fact, using a telehealth platform to connect with patients will allow them to screen way more cases throughout the year.
“Ophy Care’s telehealth solution and EMR will enable PCRF to do pre-screening and post-ops for the missions via telehealth. Pre-screening will help PCRF in allocating time to the right patients. Post-ops will enable the best and continuous care, which has been missing from short-term missions,” explained Shah.

Then, of course, the EMR technology will make it incredibly straightforward and quick to store and organize data for all these patients, which will be easily accessible from any part of the world.
Above all, an EMR will enable PCRF to have data of thousands of patients in one place to triage the best care possible and keep track of the entire care plan of a patient.
What is PCRF?
Palestine Children’s Relief Fund (PCRF) is a non-political and non-profit organization based in the US that is concerned with providing specialized medical care to children in the Middle East, regardless of their nationality, race, or political affiliation.
The organization was officially founded in 1992. However, the idea of PCRF was born a few years before that. It all started when Steve Sosebee — founder and president of PCRF — was working in the Middle East as a news writer. Sosebee came to know about two siblings who were severely injured due to a bomb thrown at their family. The ten-year-old boy, Mansour, lost his right arm and both his legs, while his sister, Sabah, needed orthopedic bone-lengthening surgery.
Neither the family could afford the expensive treatment, nor were there any hospitals providing such medical services at the time. Sosebee was determined to help these children and get them the healthcare they deserve. He used every resource and managed to bring Mansour and Sabah to Ohio in May 1990. The children stayed in the US for the next several months, getting operated and treated by experts. When they returned to their family, they both could walk again.
In a recent article on his personal blog, Sosebee wrote about his meeting with Nizar El Barky during his visit to Palestine in September 2022. Nizar is the first case he took out of Gaza in 1992. It was before PCRF was officially registered. Nizar is a triple amputee. Meeting him after three decades, Sosebee discovered he is a family man now. He has kids, and he still walks.

These are just two of the examples of how PCRF changes people’s lives in the conflict-hit region of the Middle East. Over the last three decades, PCRF has helped tens of thousands of beneficiaries, sponsored several hundred medical missions, and founded multiple healthcare departments in Gaza and West Bank.
Just in 2021 alone, despite all the restrictions due to Covid 19, PCRF supported 33 kidney transplants at Shifa Hospital; sent four children aboard for specialized medical treatment; provided surgical treatment to 834 patients; treated 766 children through psychotherapy; helped 109 amputees through Gaza Amputee Program.
What Does the Partnership Mean for Ophy Care’s Future?
“Our collaboration with PCRF is the true representation of our mission towards health equity. It is just the first step, Ophy Care aspires to be the leading player and go-to place for all organizations providing healthcare services in conflict-hit regions around the world,” said Shah.
Partnering with PCRF is an enormous milestone in Ophy Care’s journey. We strive to become the industry-leading software solution-providing company in the healthcare industry. Our telehealth platform can help a wide range of medical organizations and individual doctors overcome the challenges they face and achieve their mission more efficiently. You can learn more about us here.